A/Prof Paveyrecently had the pleasure of being interviewed by the Fairfax group on the Risk Factors for Bowel Cancer. See below for full article details.
Australia has one of the highest bowel cancer rates in the world, with 15,253 people diagnosed with bowel cancer in 2014.
After lung cancer, bowel or colorectal cancer (cancer of the large intestine or rectum) is our second biggest cancer-related killer, responsible for 4,346 deaths in 2015.
“Australia has a growing overweight and obese population. Along with insufficient physical activity, dietary factors and high tobacco and alcohol consumption rates, these factors contribute to the high rate of bowel cancer,” said Sydney-based Gastroenterologist A/Prof Pavey. Non-modifiable risk factors, including genetic predisposition also play a role, he said.
Diet and Lifestyle
“The first thing I tell my patients is to stop smoking and to reduce alcohol consumption,” A/Prof Pavey said.
“For men that means no more than two standard drinks a day, and for women no more than one.” 100 millilitres of wine equates to a standard drink (10 grams of alcohol), but an average restaurant serve is 150 millilitres.
Although not entirely clear what makes red meat carcinogenic (cancer-promoting), the link between its consumption and bowel cancer incidence is evident, A/Prof Pavey said.
“People should eat no more than 100 grams of lean red meat per day”; that’s a palm-sized steak the thickness of a deck of cards, and ideally not barbecued.
“We should be avoiding charred meat, and processed meats like salami and sausages.”
A diet rich in fibre from fruit, vegetables and whole grains however is likely to reduce bowel cancer risk, A/Prof Pavey said.
“Fibre promotes a regular bowel habit. The theory is this allows for less contact between foods and potential carcinogens with the bowel lining.”
Non-Modifiable Risk Factors
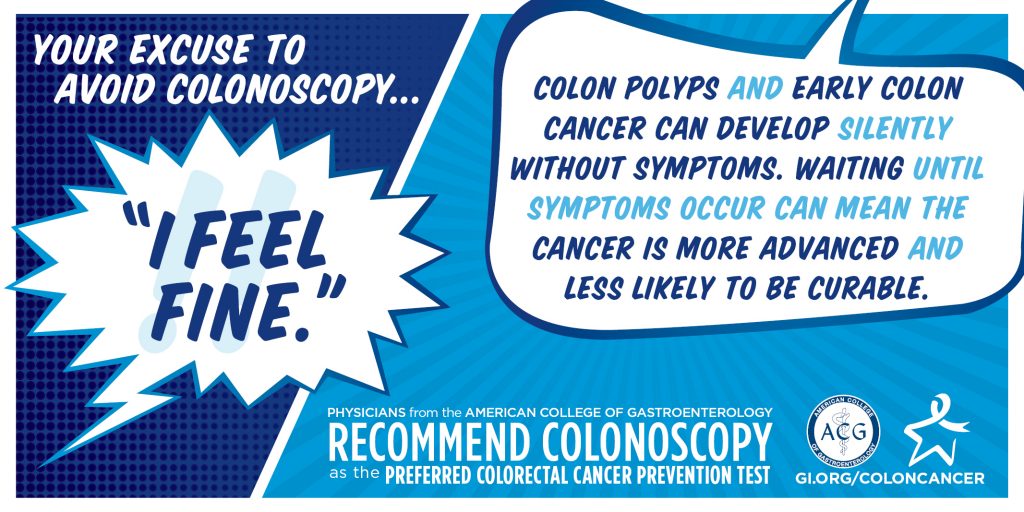
“Bowel cancer incidence goes up significantly from age 50,” A/Prof Pavey said. “That’s the stage when the screening program kicks in and becomes so important.”
The National Bowel Cancer Screening Program distributes kits to detect blood in the stool to 50 to 74-year-olds every two years.
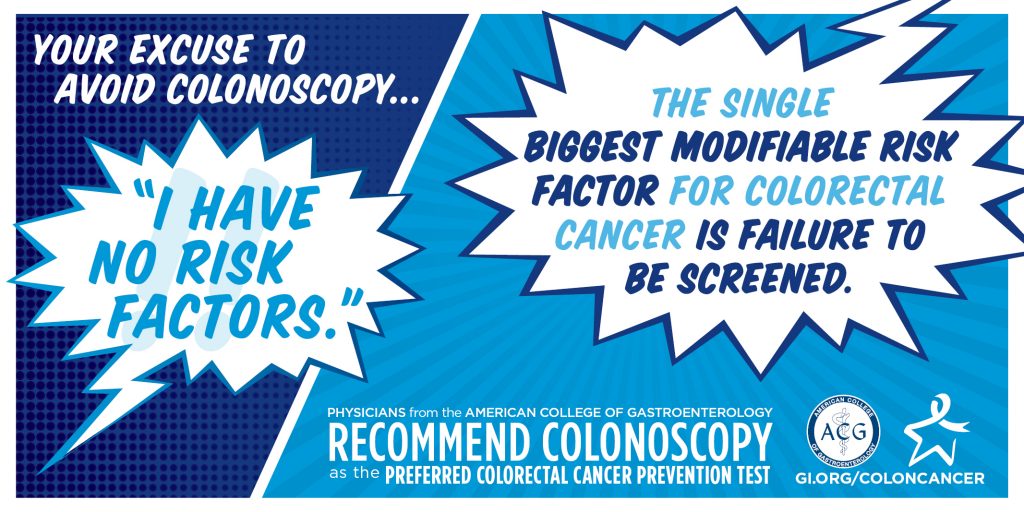
“Patients are at higher risk of developing bowel cancer if there is a family history of bowel cancer or bowel polyps (pre-cancerous lumps). They should be screened earlier and more frequently, as should those with an inflammatory bowel disease history, such as Crohn’s disease or ulcerative colitis.”
Treatment
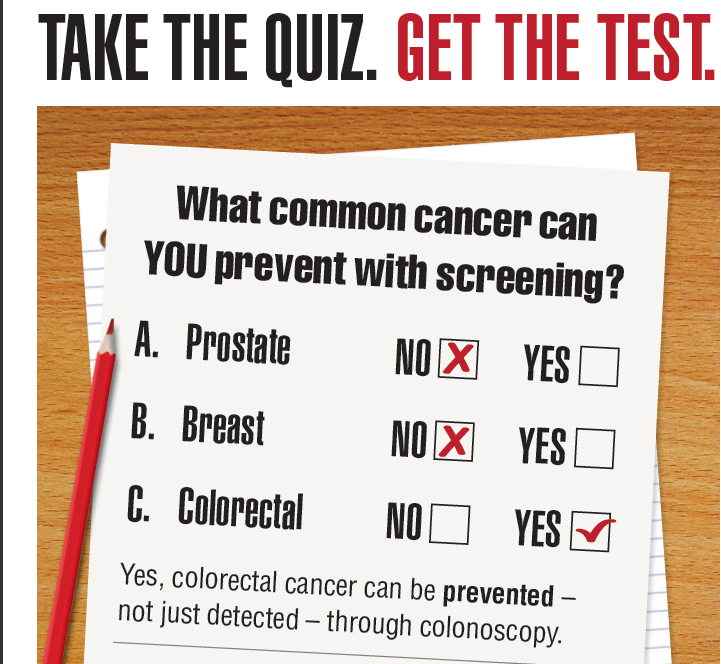
“If a polyp or growth in the bowel that may be an early cancer is found, we can remove it at the time of colonoscopy, following a positive faecal occult blood test (where traces of blood are found in the stool). That may be all that is required,” A/Prof Pavey said.
“In more advanced cases where the cancer has grown too deep into the bowel wall, patients might require surgery, and chemotherapy or radiotherapy.”
Early detection is key
There are two actions every individual should take, says A/Prof Pavey said.
“One, be aware of those modifiable (lifestyle) risk factors, and two, participate in screening from age 50, because often there are no symptoms.
“Patients should discuss with their doctor any bleeding from the bowel, changes in bowel habit, unexplained weight loss or severe abdominal pain.
“Fewer than 39 per cent of eligible Australians over age 50 complete the National Bowel Cancer screening kit. This means we are potentially missing the early detection of some treatable cancers. Unfortunately, NSW has one of the lowest participation rates at only 36 per cent.
“If we can detect bowel cancer early, 90 per cent of patients will have a good outcome.”